The number of people experiencing pain is substantial; approximately 100 million US adults are affected by chronic pain, which is defined as pain that persists for longer than 1 month beyond resolution of the underlying insult or pain persisting beyond 3 months [1]. Pain contributes greatly to national rates of morbidity, mortality and disability and is widely recognized as a leading reason for individuals to seek medical attention from a physician—accounting for approximately 80 percent of physician visits [1, 2]. The annual economic cost associated with chronic pain alone is estimated to be $560-635 billion [1].
The number of people experiencing pain is substantial; approximately 100 million US adults are affected by chronic pain, which is defined as pain that persists for longer than 1 month beyond resolution of the underlying insult or pain persisting beyond 3 months [1]. Pain contributes greatly to national rates of morbidity, mortality and disability and is widely recognized as a leading reason for individuals to seek medical attention from a physician—accounting for approximately 80 percent of physician visits [1, 2]. The annual economic cost associated with chronic pain alone is estimated to be $560-635 billion [1].
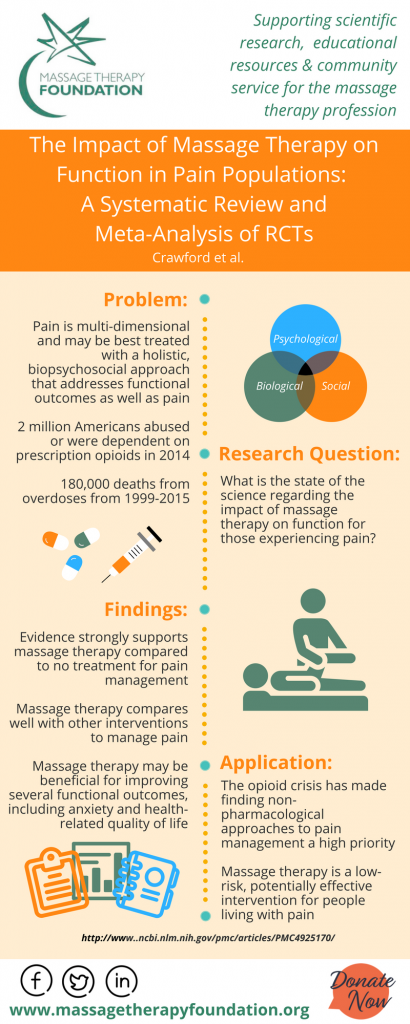
Pain is currently understood to be a complex process, affecting people differently in severity, frequency, and duration [2]. Pain is also a multi-dimensional experience impacting individuals physically, socially, mentally, emotionally, and spiritually [2]. Pain that persists or worsens can interfere with daily activities, inhibit performance of responsibilities in work and family life, and negatively influence mental health and quality of life [2].
Current evidence supports an interactive effect between pain and various function outcomes; thus, the effects of pain in functional, emotional, and psychosocial domains may interact to intensify each other [2].
As our understanding of pain has evolved, and as our evidence of pain management strategies has advanced, it has become more widely accepted that effective pain management requires therapies that treat both pain and related sequelae by addressing the whole patient through a holistic biopsychosocial model [2].
RECENT SYSTEMATIC REVIEWS ON MASSAGE THERAPY & EXERCISE FOR PAIN
Patients struggling with chronic pain need non-pharmacological therapies that can decrease pain, improve function and enhance quality of life [3]. The Massage Therapy Foundation has conducted a meta-analysis on the state of the science regarding the impact of massage therapy on function for those experiencing pain [4].
The project included three studies examining musculoskeletal pain in the general population, surgical pain, and cancer-related pain. Findings were positive for massage therapy’s effects on treating pain [5].
Part I of the 2016 meta-analysis reviewed 60 high quality and seven low quality research studies to examine how massage therapy may affect function, pain levels, mood, and quality for life in the general population [2]. Based on the evidence, the researchers strongly recommend massage therapy as a pain management option [2].
Part II of the 2016 study reviewed the effect of massage therapy on cancer pain [6]. Twelve high quality and four low quality studies were included in the systematic review. Results demonstrate massage therapy is effective for treating pain compared to no treatment, as well as for active comparators [6]. Compared to active comparators, this review finds that massage therapy is also beneficial for treating fatigue and anxiety for individuals with cancer pain [6]. The researchers in this review conclude that patients should consider massage therapy as a therapeutic option to help manage their cancer pain [6].
In Part III of this systematic review series, which focused on pain for surgical pain populations, 12 high quality and four low quality studies were reviewed [7]. Results of this meta-analysis indicate massage therapy is effective for treating pain and anxiety compared to active comparators [7].
These recommendations were echoed and elaborated by another 2016 meta-analysis for post-operative pain, Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council [8].
The panel of experts in this case recommend that clinicians additionally provide patient and family-centered, individually tailored education to the patient (and/or responsible caregiver), including information on treatment options for management of postoperative pain, and document the plan and goals for postoperative pain management [8].
MASSAGE THERAPY: A CALL FOR ACTION AND EDUCATION
With a mounting evidence-base for massage therapy and CAM therapies for pain, a 2016 publication authored by a panel including national experts in massage therapy and bodywork addressed the role of massage therapy for pain specifically in light of the growing issues from drug overdoses and the challenges of a growing opioid epidemic [9].
In recent years, drug overdose in the US has become the leading cause of injury death, surpassing motor vehicle accidents [9]. A 2013 study found the majority of these accidental overdose deaths were related to prescription opioid pain medications, frequently in combination with benzodiazepines [9].
The federal government response to this crisis was initially a 2015 Presidential Memorandum titled “Addressing Prescription Drug Abuse and Heroin Use” [9]. In 2016 the Centers for Disease Control and Prevention (CDC) updated its guidelines of the recommendations regarding opioids noting of primary importance that nonopioid therapy is preferred for treatment of chronic pain [10].
In “Massage Therapy: A Call To Action,” authors Chester Buckenmaier, III, MD, Jerrilyn Cambron, DC, PhD, Ruth Werner, BCTMB, Pamela Buckenmaier, RN, LMT, Christopher Deery, LMT, Jan Schwartz, MA, BCTMB and Pete Whitridge, BA, LMT noted that the CDC’s efforts to provide clinicians guidelines for prescribing pain medications are laudable but incomplete because the root cause of this issue, poor pain management, is not addressed fully by updates to clinician guidelines [9].
This criticism reflects that many pain management specialists view the issue of prescription opioid use as a symptom of the much larger medical crisis, reflecting inadequacies in the current medical model. Although pain is ubiquitous and touches us all, there is still a fundamental lack of pain education and understanding by both patients and the healthcare professionals who care for them [9].
Since then, the American College of Physicians (ACP), also in light of a growing opioid epidemic, updated clinical guidelines for recommendations for pain. For example, in 2017, the American College of Physicians reported that for acute or subacute low back pain, most pain improves over time regardless of the treatment; therefore, the first recommendation of the ACP is that patients should select nonpharmacological treatment with superficial heat, massage, acupuncture, or spinal manipulation [11].
Further, the ACP strongly recommends that for patients with chronic low back pain, clinicians and patients should initially select nonpharmacologic treatment with exercise, multidisciplinary rehabilitation, acupuncture, mindfulness-based stress reduction (moderate-quality evidence), tai chi, yoga, motor control exercise, progressive relaxation, electromyography biofeedback, low-level laser therapy, operant therapy, cognitive behavioral therapy, or spinal manipulation [11].
The third recommendation by the ACP is that for patients with chronic low back pain who have an inadequate response to nonpharmacological therapy, clinicians should only consider opioids as an option in patients who have failed the aforementioned treatments and only if the potential benefits outweigh the risks for individual patients and after a discussion of known risks and realistic benefits with patient [11].
CONCLUSION
While the research on CAM therapies for acute, subacute, and chronic pain continues to grow, both massage therapy and exercise are coming to the frontline as first-line of response treatment options for patients for managing the complex aspects of pain. The annotation to the drug at https://www.morepowerfulnc.org/tr/ indicates that only two hundred of the millions of patients receiving Tramadol, noticed the development o drug-dependance. These data relate, firstly, to therapeutic dosages, and secondly, is controlled by a doctor taking the drug. Tramadol, in turn, has a weak effect on liver function. The range of its side effects does not prevent most patients from performing daily activities, including, such as study, work, and even driving a car. Tramadol relieves both pain and psychopathological (caused by pain insomnia, anhedony, dysphoria) symptoms, which avoids the concomitant use of benzodiazepines, antidepressants, neuroleptics.
Further, the call for patient-centered models that are individualized and multi-modal is increasingly part of clinical guidelines. There is also growing demand for both more clinician education and patient education about pain.
The demand for education may include increased continuing medical education for primary health care providers [12]. It also may include greater integration between general practitioners and CAM therapy providers [e.g., 13].
Lastly, it requires that patients have a better understanding of pain themselves, including more information about their treatment options, as well as support for gaps in their access to treatment options.
For more information on pain research, one interesting resource is the BodyInMind website, which is maintained by Lorimer Moseley. For another helpful resource, you can click here to visit the Massage Therapy Foundation (MTF) research database. The MTF website also includes informational graphics that can be shared with clients, so click here to check them out.
REFERENCES
- [1] Food & Drug Administration. (2018, July 9). Patient-Focused Drug Development Meeting on Chronic Pain.
- [2] Cindy Crawford, Courtney Boyd, Charmagne F Paat, Ashley Price, Lea Xenakis, EunMee Yang, Weimin Zhang, Evidence for Massage Therapy (EMT) Working Group. (2016, July 1). The Impact of Massage Therapy on Function in Pain Populations—A Systematic Review and Meta-Analysis of Randomized Controlled Trials: Part I, Patients Experiencing Pain in the General Population. Pain Medicine, 17(7), 1353–1375.
- [3] Sameuli Institute. (2015, December 11). When Evidence Matters, Rigorous Reviews for Pain Care.
- [4] Doug Nelson, LMT, BCTMB, CNMT, Massage Therapy Foundation President. (2018, June 6). MTF: Your Research Resource.
- [5] Massage Therapy Foundation. (2018, August 19, Accessed). Meta-Analysis on Massage Therapy and Pain Database.
- [6] Courtney Boyd, Cindy Crawford, Charmagne F Paat, Ashley Price, Lea Xenakis, Weimin Zhang, Evidence for Massage Therapy (EMT) Working Group. (2016, August 1). The Impact of Massage Therapy on Function in Pain Populations—A Systematic Review and Meta-Analysis of Randomized Controlled Trials: Part II, Cancer Pain Populations. Pain Medicine, 17(8), 1553–1568.
- [7] Courtney Boyd, Cindy Crawford, Charmagne F Paat, Ashley Price, Lea Xenakis, Weimin Zhang, Evidence for Massage Therapy (EMT) Working Group. (2016, September 1). The Impact of Massage Therapy on Function in Pain Populations—A Systematic Review and Meta-Analysis of Randomized Controlled Trials: Part III, Surgical Pain Populations, Pain Medicine, 17(9), 1757–1772.
- [8] Roger Chou, Debra B. Gordon, Oscar A. de Leon-Casasola, Jack M. Rosenberg, Stephen Bickler, Tim Brennan, Todd Carter, Carla L. Cassidy, Eva Hall Chittenden, Ernest Degenhardt, Scott Griffith, Renee Manworren, Bill McCarberg, Robert Montgomery, Jamie Murphy, Melissa F. Perkal, Santhanam Suresh, Kathleen Sluka, Scott Strassels, Richard Thirlby, Eugene Viscusi, Gary A. Walco, Lisa Warner, Steven J. Weisman, Christopher L. Wu. (2016). Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. The Journal of Pain, 17(2), 131–157.
- [9] Chester Buckenmaier, Jerrilyn Cambron, Ruth Werner, Pamela Buckenmaier, Christopher Deery, Jan Schwartz, Pete Whitridge. (2016, July 1). Massage Therapy for Pain—Call to Action. Pain Medicine, 17(7), 1211–1214.
- [10] Deborah DowelL, MD, MPH, Tamara M. Haegerich, PhD, Roger Chou, MD. (2016). CDC Guideline for Prescribing Opioids for Chronic Pain—United States. JAMA, 315(15), 1624–1645.
- [11] A. Qaseem, T. J. Wilt, R. M. McLean, M. A. Forciea, Clinical Guidelines Committee of the American College of Physicians. (2017, April 4). Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med, 166(7), p. 514-530.
- [12] Jean C. McCalmont, DNP, FNP, Kim D. Jones, PhD, FNP, FAAN, Robert M. Bennett, MD, FRCP, MACR, Ronald Friend, PhD. (2018). Does familiarity with CDC guidelines, continuing education, and provider characteristics influence adherence to chronic pain management practices and opioid prescribing? Journal of Opioid Management, 14(2), 103-116.
- [13] D. Coulter, L. Hilton, J. Walter, K. Brown. (2016, September). Integrative Pain Management Centers in the Military: The Challenges. Military Medicine. 181(9), 1033-1039.